Public Resources
Public Resources
PPE for First Receivers at Hospital-Based Patient Decontamination Events
A. Chemical Protective Suit for First Receivers
According to OSHA, “The appropriate employee training and PPE selection processes are defined in applicable OSHA standards. An employee’s role and the hazards that an employee might encounter dictate the level of training that must be provided to any individual first receiver. PPE selection must be based on a hazard assessment that carefully considers both of these factors, along with the steps taken to minimize the extent of the employee’s contact with hazardous substances.”3
Personnel trained to the OSHA hazardous materials operations level are the only individuals, besides hazardous materials technicians, that should be permitted in the warm zone. Once in the warm zone, they should only be permitted to conduct defensive operations, to include patient decontamination reduction operations. It is unlikely that a hot zone will be established at a hospital, unless of course the hazardous materials event occurred there. Work activities in a warm zone will mainly consist of patient screening, security operations, triage and traditional decontamination operations. In order to conduct these activities safely, the type of chemical protective suit chosen is as equally important as the training received.
B. PAPR Respiratory Protection
OSHA recommends at a minimum that PPE for first receivers includes: “A PAPR with an assigned protection factor (APF) of 1,000, a chemical-resistant protective garment, head covering if it is not already included in the respirator, a double layer of protective gloves, and chemical-protective boots. An employee wearing a respirator that offers a protection factor of 1,000 will breathe air that contains no more than 1/1,000 (or 0.1 percent) of the contaminant level outside the respirator.”4
The recommendations for the use of PPE by hospital first receivers have changed significantly in recent years. Many hospitals originally invested in Self-Contained Breathing Apparatus (SCBA) technology after 9/11. Additionally, OSHA has deemed in a Letter of Interpretation that “hospital staff members who decontaminate a patient at the hospital are removed from the site of the emergency and the point of release,” and “OSHA does not require hospital staff members who decontaminate patients to wear Level B respiratory protection.” 5Note: Even given this OSHA Letter of Interpretation, PAPRs should technically not be used in an unknown hazardous materials environment, and should never be used when the assigned protection factor of 1,000 is not sufficient for the hazardous material present in the work environment.
Many hospitals in Massachusetts with patient decontamination programs have converted to the PAPR style respirator. PAPRs are fairly simple to use, maintain, and service. They provide a greater field of vision and allow the user to stay in the warm zone longer than if they were operating in an SCBA, which limits the wearer to the amount of air in their cylinder which in most cases is roughly 30 – 60 minutes.
When fully charged, PAPR batteries should power the PAPR blower unit for anywhere from two to fourteen hours, depending on the manufacturer. And unlike SCBA bottles which should never be changed during the course of a real-world hazardous materials event, PAPR batteries may safely be changed in a hazardous materials environment without putting the wearer in danger.
What is the difference between respirators and surgical masks?
There is a significant difference between certain respirators. Understand the difference by clicking on the video below:
U.S. Department of Labor/OSHA: The Difference between Respirators and Surgical Masks
C. PAPR Components
First generation PAPR blower units were originally attached to a rugged, plastic belt which could be adjusted to the wearer, however, newer models configurations include a comfortable backpack configuration ensemble. The following is a list of common PAPR components:
- respiratory hood
- hood apron
- PAPR blower unit
- blower holder (belt or backpack configuration)
- breathing tube
- PAPR battery
- air flow tester
- NIOSH-approved CBRN Canisters
DelValle Institute for Emergency Preparedness: 360° View of the Powered Air Purifying Respirator
D. PAPR Maintenance, Care and Storage
Click on the video below for detailed information on the proper maintenance, care and storage of PPE:
U.S. Department of Labor/OSHA: Maintenance and Care of Respirators
The items that make up the PAPR, including all related PPE ensemble items, must be properly stored and maintained by trained individuals according to the manufacturer’s instructions in order for the equipment to remain functional and provide the expected level of safety when needed. Not adhering to the manufacturer’s storage and maintenance guidance could negate any warranties or exonerate the manufacturer from possible liability if the equipment were to not perform as stated, or simply fail. A worst case scenario could result in a worker’s death.
PPE ensembles, including PAPRs, must be stored in a secure, dry, climate controlled area of the hospital free of dust, damaging chemicals, and sunlight. A plan should be made to rotate PPE stock, verify and track expiration dates, and when necessary, charge PAPR and other batteries. Note: Once removed from its original packaging, chemical resistant suits and gloves have a specific time period stated by the manufacturer for which they will remain safe to use. Once this time has elapsed, the equipment must either be discarded or designated as training equipment only.
Using PPE that has been removed from its original packaging after the specific time stated by the manufacturer could significantly endanger a worker’s health and safety. Additionally, any equipment that has not been removed from its original manufacturer’s packaging must also be discarded or designated for training use if the manufacturer warranty has expired. Note: Many chemical protective suits, gloves, footwear, canisters, filters and most respirators have a specific shelf life.
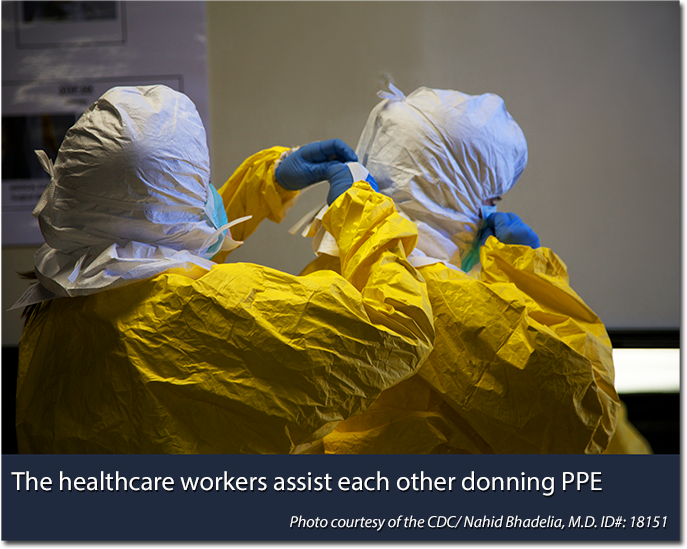
Concerted efforts should be made to house the equipment as close to the planned patient decontamination area of operations as possible. Doing so will not only speed the movement of the first receiver to the area of operations; it will also significantly decrease their overall level of fatigue. Workers should be familiar with the donning and doffing area, and how to access the equipment regardless of time of day.
E. PAPR Inspection Procedures
The OSHA standard requires “respirators designated for use in an emergency situation are to be inspected at least monthly and in accordance with the manufacturer's instructions, and checked for proper function before and after each use.” – OSHA Technical Manual, Section VIII: Chapter 2
Inspect for:
- Damage to straps and connection points
- Breathing tube degradation
- Equipment free of holes, tears or punctures
- Face piece not cracked or distorted
- Battery fully charged
- Cartridges are properly sealed and the service life has not been exceeded
- Successful air flow test
F. N95 Respirators
N95 respirators are the most common type of particulate respirators used in industry today. FDA-cleared N95 respirators specifically for the health care industry are referred to as surgical respirators.
Contrary to popular belief, N95 respirators are not tested against specific chemicals, biological agents or radioactive contamination, but instead are tested using only non-hazardous airborne particles. The reason for the N95 designation is due to the fact that during testing, they blocked at least 95% of all test particles. Click here to see a list of NIOSH-approved N95 respirators, listed alphabetically by manufacturer.
G. N95 Respirator Facts
- manufacturer meant to help block large-particle droplets, splashes, sprays or splatter;
- all FDA-cleared N95s are considered single-use;
- fit testing is mandatory;
- even a properly fitted N95 doesn't eliminate the risk of illness or death;
- N95s are not designed for children or adults with facial hair;
- not resistant to oil.
N95 Respirator Seal Checks
OSHA: How to Perform a User Seal Check with an N95 Respirator
Use of Respirators in Healthcare Settings
OSHA: Respiratory Protection for Healthcare Workers Training (2011)
Note: Although some pieces of a chemical protective ensemble typically used during a patient decontamination scenario are also utilized in various other hospital PPE ensembles, PAPRs are not always used in biological pathogen cases, such as treating patients infected with Ebola hemorrhagic fever (EHF). As more information about these types of deadly diseases is discovered, federal recommendations are often updated in regards to PPE modifications. For more detailed information on PPE for EHF specifically, click here for OSHA’s most updated information on Ebola.
« Previous | Topic Home | Next »
References:
3 OSHA Website. (2005, January) OSHA Best Practices for Hospital-Based First Receivers of Victims from Mass Casualty Incidents Involving the Release of Hazardous Substances. Retrieved from: https://www.osha.gov/dts/osta/bestpractices/html/hospital_firstreceivers.html
4 OSHA Website. (2005, January) OSHA Best Practices for Hospital-Based First Receivers of Victims from Mass Casualty Incidents Involving the Release of Hazardous. Retrieved from: https://www.osha.gov/dts/osta/bestpractices/html/hospital_firstreceivers.html

